Help Sean Turner Fight Testicular Cancer
Hello everyone,
I’m here to do something that is uncomfortable for me; to ask for help. I’m creating this page as a both a method of sharing my story for all those who are interested (and so that I don’t have to repeat it individually to everyone, although I’m open to answering questions and sharing more to those who reach out to me) and as a vessel for those with the ability and desire to provide financial support. In my day-to-day life, I tend toward limited disclosure of personal information, even to close friends and family, so this topic of discussion is one that has been difficult to become accustomed to. Even so, there is an element of catharsis in creating and sharing a written expression of my experiences, regardless of the initial discomfort, so those reading this should feel at ease that this was actually a helpful exercise in personal reflection and emotional processing and not a forced disclosure of personal information.
My Story
I first noticed testicular pain/discomfort around November 2024, to the best that I can remember. The pain was intermittent, and not particularly localizing. Imagine a diffuse pain/pressure/feeling of heaviness in the groin/lower abdomen. A kind of sensation that could easily be dismissed as resulting from “sitting in a weird position” or “muscle soreness.” The discomfort did eventually become concerning enough to warrant a visit to an urgent care clinic before traveling for the holidays in December 2024. That clinic misdiagnosed it as a varicocele (enlargement of veins in the scrotum) and prescribed ibuprofen. They did not perform any diagnostic tests and were pretty dismissive of it being a serious concern. However, they did provide the disclaimer that should the pain not improve in a few weeks, I should follow up with a urologist. I pretty quickly after that visit set up an appointment with a urology provider, the soonest available being three months out.
I first met with a Physician Assistant in the department of Urology at the University of Texas – San Antonio on March 17, 2025. On physical examination, she noticed of a left-testicular mass that was painful to palpation; something that I had also noticed in the preceding months. A testicular mass is never normal and always concerning for testicular cancer, although the most common forms of testicular cancer often present as a painless lump. The provider ordered a STAT ultrasound, which I obtained the next day, which revealed a lesion suspicious for left testicular malignancy. That provider promptly referred my case to a urologic surgeon/oncologist who ordered additional blood tests for common tumor markers (one of which-alpha fetoprotein or AFP-was slightly elevated) and recommended surgical removal of the testicle as soon as possible.
Surgery was completed on March 26, 2025. Pathological analysis of the lesion classified the tumor as primarily embryonal carcinoma (think Lance Armstrong – but without the performance enhancing drugs). I recovered from surgery without complications and began a series of follow-up diagnostic tests to determine proper staging and inform treatment planning. This type of cancer has a prototypical pattern of metastasis that usually involves initial spread to the retroperitoneal lymph nodes (the lymph nodes located in the back of the abdomen around the major blood vessels), the lungs, liver, and brain. If the spread is limited to the lymph nodes, surgical treatment to remove those lymph nodes (retroperitoneal lymphadenectomy or RPLND) can be considered. There is also an effective combination of chemotherapy drugs (Bleomycin, Etoposide, and Cisplatin) that can be used for a variety of reasons, including metastatic disease outside of the lymphatic system (spoiler alert – this becomes relevant later). Otherwise, I would enter an active surveillance stage consisting of repeated diagnostic tests at regular intervals to detect changes early, since there is high risk of metastasis in this cancer.
The diagnostic workup to determine the presence and stage of metastatic disease includes repeated blood tumor marker analyses and CT scans of the chest and abdomen. My blood markers were normal post-surgery and my initial CT scans conducted on April 16, 2025 did not show overt evidence of metastases, but did show some, perhaps, mildly enlarged lymph nodes. The determination of whether lymph nodes are concerning for cancer spread based on CT imaging is largely based on size, with there being individual variability in what is “normal.” Given that I was already known to have a type of cancer with a predisposition for spread to that region, the doctor decided to perform a repeat CT scan in a shorter interval than would be typical, to determine if the size of the lymph nodes was stable. Interestingly, given that my chest CT did not show any concerning signs, he only ordered the abdominal scan at follow up. I completed next abdominal scan on June 10, 2025. The good news was that the retroperitoneal lymph nodes that we were concerned about looked about the same and were not overtly concerning for cancer, however, it was incidentally noted that there were “new nodules in the bilateral visualized lung bases, the largest is in the left lower lobe measuring 1.5 cm.” An abdominal CT scan captures just the lower portion of the lungs as it is focused on the structures lower in the abdomen, so it was an unexpected finding to notice changes in my lungs. My doctor reviewed the scans the same day and informed me that this is concerning for lung metastases and that I would need to have a chest CT and be evaluated by the medical oncology team, since this forces the treatment options directly to chemotherapy.
The follow up chest CT, unsurprisingly, confirmed what was noted in the abdominal CT. I had an initial appointment with medical oncology on June 11, 2025 with the tentative plan to undergo three cycles of bleomycin, etoposide, and cisplatin (BEP – cisplatin also goes by the name Platinol as it is platinum based, hence the “P”) chemotherapy. This is pending lung function tests to make sure my lungs are strong enough for the bleomycin and various lab work and insurance approval stuff.
Other Life Circumstances
While there is certainly no “good” time for a cancer diagnosis, it does seem like this came at a pretty inopportune moment. I am currently a psychology intern at the South Texas Veterans Health Care System in San Antonio, TX. For those pursuing a Ph.D. in psychology (like me) the internship year represents the final year of graduate training. I engage in full-time clinical work, under supervision, while simultaneously completing the requirements of my graduate program, like completing my dissertation. It’s an interesting system in which I am a full-time intern in San Antonio but still a student at the University of Florida, meaning I still pay tuition to the university. That is one of many expenses that have quickly outpaced my internship stipend over the last year. In addition to the normal living expenses of rent, car payments, insurance, groceries, car repairs, I can now add thousands of dollars in medical bills to my docket. It is also unfortunate timing that my current lease ends on July 7th and I had already decided that I was not going to renew this lease (my third-floor apartment regularly reaches 90+ degrees in the summer with the A/C running continuously), thus I also need to move. The good news is that I am staying at my current training site for a two-year fellowship that begins August 2025, so I do not have to move across the country. The bad news is that there is a 4-week break from July 11th to August 11th that I am technically not employed and therefore not paid. Prior to my health taking a turn for the worse I was donating (selling) my blood plasma for money to make ends meet, although now nobody would pay a dime for my plasma. While in school, I drove as an Uber driver on nights and weekends to supplement my income. I won’t be able to do that now. I was also planning on staying in a friend’s apartment during the break to save money, although now that would require moving all my belongings, twice, in the timeline of receiving chemotherapy, which I do not think will be a feasible option.
This diagnosis has been physically, emotionally, and financially overwhelming. I’m hopeful that my treatment will be successful and that I will reflect on this period as evidence that I can persevere and overcome any obstacles that fall in my way. But as hard as it is to admit it, I cannot complete this part of the journey on my own; neither physically, emotionally, nor financially. I am so grateful to everyone who has reached out to me with well-wishes and to offer support in whatever way they are able. While I recognize that I am not always the best at communicating or expressing my gratitude/feelings (ironic since I’m nearly a psychologist), know that I appreciate every bit of support that I receive and am deeply honored to have such a supportive network of family and friends.
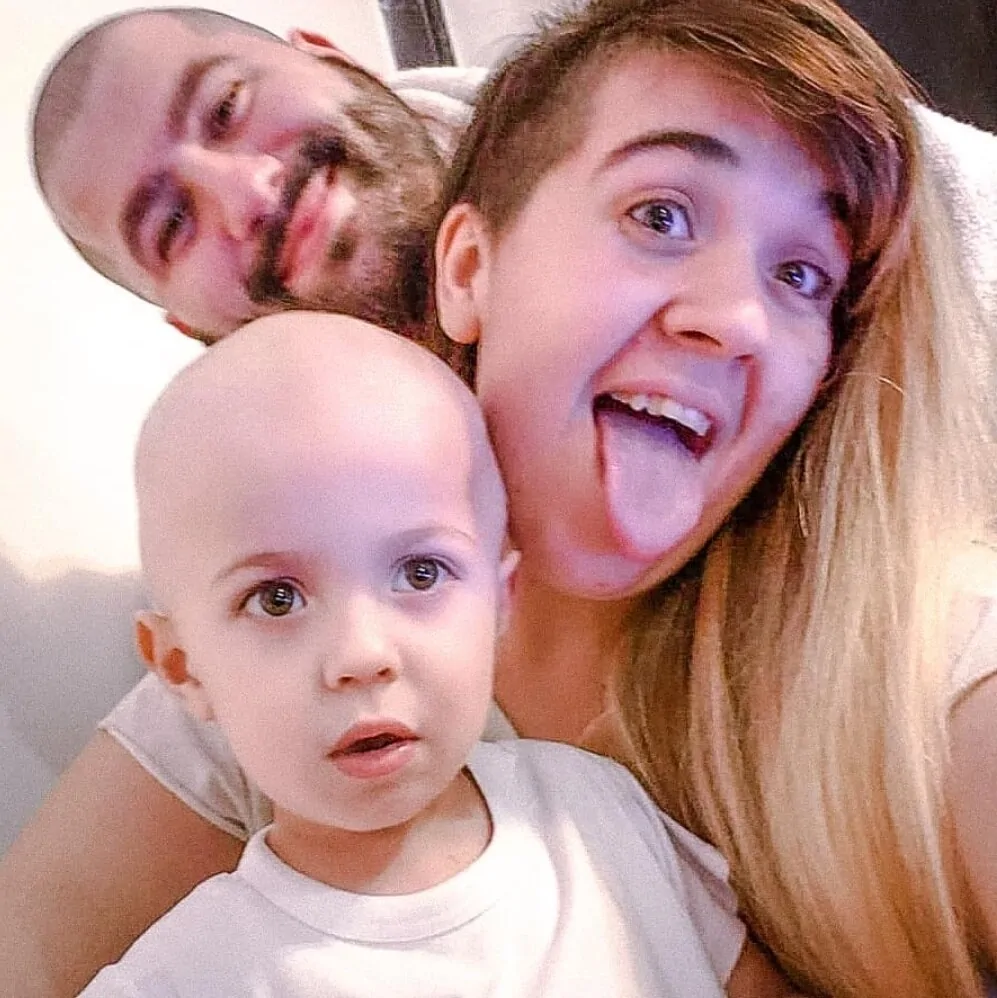
I am fortunate to feel physically-well at this stage. In fact, if I did not know about the lung nodules, I would not think there was cancer spreading throughout my body (see the photo above of me on a hike taken just prior to my diagnosis in March). I am also fortunate to be located in a city with access to world-class medical treatment. The University of Texas Health San Antonio – Mays Cancer Center is a National Cancer Institute (NCI) designated Clinical Cancer Center that is partnered with MD Anderson Cancer Center. I have the utmost respect and trust for my team of healthcare professionals and feel confident in the care that I am receiving here.
Thank you for taking the time to read my story. Your support gives me strength and motivation each day as I face new challenges and uncertainty on this journey.
With sincere gratitude,
Sean M. Turner